Connect With Us
Blog

The Importance of Biomechanics in Podiatry
Biomechanics and its related study deal with the forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
Biomechanics and its related study deal with forces that act against the body and affect things like our movement. In podiatry, biomechanics are studied to determine the movement of the ankle, toes, and the foot, as well as the forces that impact them. Podiatrists who train in this specialty are able to effectively diagnose and treat conditions that affect people’s everyday movement.
Regardless of your lifestyle, age, or any other factors, many people experience foot problems throughout their lives. Twists and turns, improper balance, and added weight are just a few of the things that can add stress to the feet. These issues can also limit our bodies’ mobility that we often take for granted. Pain in the feet and ankles can also trickle up towards the lower legs, knees, hip, and even back area. This affects the way you move around on a daily basis.
The history of studying biomechanics dates back to ancient Egypt at around 3000 B.C., where evidence of professional foot care has been recorded. Throughout the centuries, advances in technology, science, and an understanding of the human body led to more accurate diagnosis of conditions such as corns for example. In 1974, biomechanics garnered a large audience when Merton Root founded Root Lab to make custom orthotics. He proposed that corrections of certain conditions could be implemented to gain strength and coordination in the area. Due to his research, we still use his basic principle of foot orthotics to this day.
As technology has improved, so have the therapeutic processes that allow us to correct deficiencies in our natural biomechanics. Computers can now provide accurate readings of the forces, movements, and patterns of the foot and lower leg. Critical treatment options can be provided to patients now who suffer from problems that cause their biomechanics to not function naturally. The best results are now possible thanks to 3D modeling and computing technologies that can take readings and also map out what treatment will do to the affected areas.
These advanced corrective methods were able to come to light thanks to an increase in both the technologies surrounding biomechanics and also the knowledge of how they work naturally. For example, shoe orthotics are able to treat walking inabilities by realigning the posture deviations in patients caused by hip or back problems. Understanding foot biomechanics can help improve movement and eliminate pain, stopping further stress to the foot. Speak with your podiatrist if you have any of these problems.
How Seniors Can Prevent Falling

As people age, preventing falls becomes more and more important for maintaining overall well-being. Exercise plays a pivotal role in fall prevention. Activities that improve balance and strengthen your legs, such as Tai Chi, are beneficial. Lack of exercise leads to weakness, increasing the risk of falls. Regular eye and foot check-ups are essential, as poor vision raises fall risks. Certain modifications can enhance your safety at home. Remove tripping hazards, secure rugs with double-sided tape, and place frequently used items within easy reach. Install grab bars in the bathroom, use non-slip mats, and improve lighting. Lastly, wear well-fitting, supportive shoes, both indoors and outdoors. Handrails and proper lighting on staircases, both indoors and outside, contribute to a safer living environment. Review all medications, as some can cause dizziness. Discuss vitamin D supplements to enhance bone, muscle, and nerve health. Keep your podiatrist informed if balance or other foot problems are putting you at risk for falls. Additionally, it is suggested that you schedule an appointment yearly to have your feet examined by a podiatrist in addition to discussing any foot issues that may contribute to risks of falling.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
A Closer Look at Causes of Cuboid Syndrome

Cuboid syndrome, a relatively lesser known foot ailment, involves the dislocation or subluxation of the cuboid bone, which is one of the seven tarsal bones in the foot. This condition typically occurs when there is excessive stress on the foot, often stemming from activities that involve repeated impact or sudden twisting motions. Participating in high impact sports, wearing improper footwear, or sudden changes in activity levels can contribute to the misalignment of the cuboid bone. The cuboid bone sits on the outer side of the foot, forming a vital connection between the foot and the ankle. When it shifts out of its normal position, it can cause pain and discomfort along the outer edge of the foot, accompanied by swelling and limited range of motion. Recognizing the definition and understanding the causes of cuboid syndrome is essential for prompt diagnosis and appropriate management that can restore normal foot function. If you have pain in this area of your foot, it is suggested that you contact a podiatrist who can accurately diagnose whether it is cuboid syndrome and offer appropriate treatment techniques.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cuboid Syndrome
Cuboid syndrome mostly affects athletes, although it can affect non-athletes too. It is also known as cuboid subluxation or cuboid fault syndrome. This condition occurs when joints and ligaments near the cuboid bone of the foot are damaged, or when the cuboid bone itself is dislodged from its natural position. It is usually marked by pain on the outer side of the foot, which may be persistent or may come and go. Cuboid syndrome can be difficult to diagnose unless it becomes severe and more noticeable. Your doctor will likely ask questions about when the pain began and how long it has been present, and will put pressure on the cuboid bone to determine if that area is the origin of the pain.
Causes of Cuboid Syndrome
- Any repetitive stresses placed on the foot due to athletic activities are a common cause of cuboid syndrome.
- Although it develops over time, it is possible that this syndrome can occur all of sudden due to a single event or injury.
- Over-pronation can exacerbate the condition if not corrected.
Disagreements Amongst Podiatrists Regarding Cuboid Syndrome
- Some refer to it as the dislocation of the calcaneal-cuboid joint only.
- Other podiatrists see it as an injury of the ligaments located nearby, which also involves the cuboid bone.
It is very important that when you experience any kind of pain on the side of your foot, you should seek medical care right away. If a subluxed cuboid is caught early, your feet may respond well to the treatment, and you can get back into sports or other activities again as soon as the pain subsides.
Early Indicators of Foot Arthritis
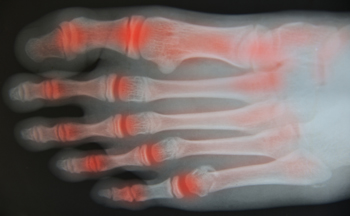
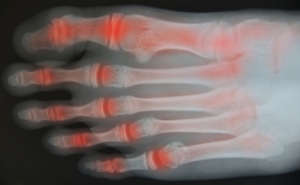
Foot arthritis, a condition affecting the joints in the feet, often begins its onset with inconspicuous signs that warrant attention. Persistent morning stiffness, particularly in the feet, can be an early red flag. Individuals may notice increased discomfort during weight-bearing activities or difficulty flexing and extending the foot joints. Swelling and warmth around the joints may accompany these symptoms, indicating inflammation. As arthritis progresses, subtle changes in foot structure or the development of bunions and hammertoes may become noticeable. Gradual limitations in range of motion may hinder daily activities. Persistent pain, even at rest, is another key signal that warrants investigation. Recognizing these initial whispers of foot arthritis allows for early intervention, potentially mitigating the impact on mobility and overall quality of life. If you have symptoms of foot arthritis, it is strongly suggested that you are under the care of a podiatrist who can effectively diagnose and offer treatment and relief options.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
Effective Stretches for Improved Heel Stability

Heel stability is an important aspect of overall balance and comfort, and it is often overlooked until you experience pain or discomfort in that area. Fortunately, there are several stretches that can help enhance heel stability and promote overall foot health. One beneficial stretch is the calf stretch. This simple exercise involves extending one leg behind you and leaning forward with the other, feeling the stretch in your calf and Achilles tendon. By keeping these areas flexible, you reduce the strain on your heel. Another effective stretch is the plantar fascia stretch. To perform this, sit down and cross one ankle over the opposite knee. Gently pull your toes back toward your shin, feeling the stretch along the arch of your foot. This stretch helps to maintain the flexibility of the plantar fascia, thus reducing the risk of heel pain. The final stretch to consider is the toe stretch. This can be done by sitting or standing and extending your toes as far as possible, then curling them under. This exercise strengthens the muscles in your feet and enhances overall heel stability. If you would like additional information about effective heel stability stretches, it is suggested that you speak with a podiatrist who can provide you with the knowledge you are seeking.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Being the backbone of the body, the feet carry your entire weight and can easily become overexerted, causing cramps and pain. As with any body part, stretching your feet can serve many benefits. From increasing flexibility to even providing some pain relief, be sure to give your feet a stretch from time to time. This is especially important for athletes or anyone performing aerobic exercises, but anyone experiencing foot pain or is on their feet constantly should also engage in this practice.
Great ways to stretch your feet:
- Crossing one leg over the others and carefully pull your toes back. Do 10-20 repetitions and repeat the process for each foot
- Face a wall with your arms out and hands flat against the wall. Step back with one foot and keep it flat on the floor while moving the other leg forward. Lean towards the wall until you feel a stretch. Hold for 30 seconds and perform 10 repetitions for each foot
- Be sure not to overextend or push your limbs too hard or you could risk pulling or straining your muscle
Individuals who tend to their feet by regular stretching every day should be able to minimize foot pain and prevent new problems from arising.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stretching Your Feet
Debilitating foot pain is a problem for many people. But just as stretching the torso can help alleviate back pain, stretching the feet can also help mend existing foot problems and prevent future ones.
The feet, as the body’s foundation, carry the body’s entire weight and can get easily strained from overexertion. Persistent sharp pain and cramping in the feet are often common concerns. Foot pain and foot problems can be due to any number of causes, and in many cases pain may be eased without medication or doctor visits. It is always a good idea, however, to first rule out any serious medical issues with a physician.
Stretching can help relax the feet and alleviate pain, but is especially important before heavy aerobic exercise. Stretching before such activities can help you avoid experiencing painful cramps or strained foot muscles. Stretches should be performed slowly and deliberately without forceful pulling. The stretch should be held for several seconds before relaxing.
A great way to stretch out and loosen up the foot muscles while sitting is to cross one leg over the other and pull the toes carefully back without overextending. Start by resting the left ankle on the right knee. With the left hand, gently flex the left foot by pulling back on the toes. Do not pull too hard; just hard enough to feel the stretch in the arch of the foot. Then point the toes of the left foot as far as you can. Rotate the motion of pointing with pulling back on the toes. This should relax and stretch the muscles on the bottom and the top of the foot. Doing this stretch ten to twenty times should bring relief. Repeat the whole process for the other foot by resting the right ankle on the left knee.
A stretch that focuses on the often injured Achilles tendon involves standing and facing a wall with your arms out and hands flat against the wall. Step back with one foot, keeping it flat against the floor. Move the other leg forward and lean toward the wall. You should feel a stretch through the back of your leg and your Achilles tendon, but do not push yourself too much. Stop when you feel a stretching sensation, and hold for 30 seconds. Ten repetitions may be done for each foot.
Stretching the feet is important for athletes or those performing aerobic exercise, but it can also help anyone with foot pain caused by poor footwear, plantar fasciitis, or long hours standing and walking. Individuals who tend to their feet by regularly stretching every day should be able to minimize foot pain and prevent new problems from arising.
Blog Archives
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021