Connect With Us

How to Know if You Have a Broken Foot

A broken foot can occur from a fall or being hit by an object. Those with osteoporosis, a bone condition often seen in older adults where bones are more likely to be weak or brittle, should be particularly careful of broken bones. Signs of a broken foot are pain, swelling, and deformity. A snap or grinding noise may be heard at the time of injury, and there may be swelling, bruising, or tenderness near the injured area. It will also likely be painful to bear weight on the affected foot. If you suspect a break, elevate the foot, and make an appointment with a podiatrist who can evaluate the injury and determine the correct treatment for you.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Changing Shoes May Provide Relief for Morton’s Neuroma
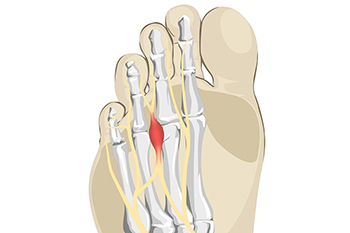
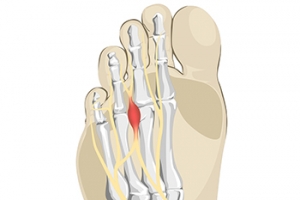
The digital nerve in the feet is defined as the nerve that transports sensations to and from the toes. If this nerve becomes irritated or inflamed, it can cause severe pain and discomfort, often causing difficulty in walking. Morton’s neuroma is a foot condition that affects women more than men, and this can be a result of frequently wearing high heels. These types of shoes generally have limited room for the toes to move freely in, and the digital nerve can become compressed. It is located between the third and fourth toes, and the sensation that is felt can be likened to having a marble in the shoe. Additional symptoms can include a numbing feeling, and pain may occur in the ball of the foot. Relief is often found when high heels are eliminated, and it is suggested to wear shoes that are flat or have a lower heel. If you are afflicted with Morton’s neuroma, please speak to a podiatrist who can guide you toward the correct treatment options, which may include surgery for repair or removal of the nerve.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Anyone Can Get Athlete’s Foot

The foot condition known as athlete’s foot was originally named as a result of athletes getting this type of fungal infection. Despite this fact, it is common among the general population and can be quite uncomfortable. The fungus that causes this condition lives in warm environments and enters the body through small cracks in the skin. Public swimming pools, shower room floors, and locker rooms are common areas where this fungus is found. The symptoms that many people experience with this ailment include dry skin that becomes red and inflamed, and in severe cases, blisters may develop between the toes. Proper preventive methods consist of washing the feet, followed by drying them completely. Additionally, it is beneficial to wear appropriate shoes, such as flip-flops or water shoes, while in these types of areas. Many people seek expert medical attention that can provide relief, and it is suggested that you confer with a podiatrist who can prescribe the correct medications for athlete’s foot.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
Club Foot Is Treatable

Club foot is a condition that begins when the baby is inside the womb. It is considered to be a rare foot condition and is noticeable as the feet turn in and point down. It happens as a result of a short Achilles tendon and can affect one or both feet. Club foot is generally not painful to babies despite the difficulty in walking if it is not treated. An ultrasound can be performed during the pregnancy, and it can give the parents the opportunity to speak with their doctor about specific treatment methods. A common treatment is referred to as the Ponseti method, and this provides gentle manipulation that stretches the feet into a better position. This is followed by having the baby wear a cast, and the method is repeated approximately every eight weeks. Minor surgery may be necessary to perform on the Achilles tendon when the feet have straightened out, and this can be helpful in loosening this tendon. If you have questions about club foot, it is strongly advised that you seek the counsel of a podiatrist who can perform the necessary treatment options that can benefit your child.
Some foot conditions may require additional professional care. If you have any concerns, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.