Connect With Us

Treatment for Plantar Warts

A plantar wart, which is a growth on the sole of your foot, is caused by exposure to the human papillomavirus, or HPV. Although this type of infection is more common among children and young adults, it can affect anyone. You might wonder how you end up with this unwelcome visitor. It's simple, the infection is caused by direct contact with the virus through a break in your skin. Sometimes, it can take months after exposure for a plantar wart to appear. The wart often starts as a small, rough patch on your foot's sole but can expand over time. These growths disrupt the usual skin lines on your feet and might display tiny black dots due to clogged blood vessels. Treatment options vary based on how the warts bother you. Salicylic acid treatments may or may not be effective. More advanced treatment includes the application of liquid nitrogen to freeze the skin, though this process can cause discomfort and may take several applications. If you think you may have a plantar wart, especially if it becomes painful or shows signs of infection, it is suggested that you make an appointment with a podiatrist. This qualified foot doctor can evaluate the problem and suggest a proper course of treatment.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
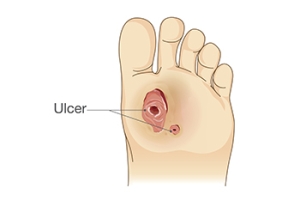
Stages of Diabetic Foot Ulcers
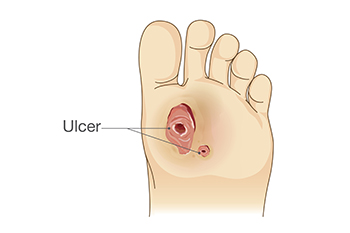
Diabetic foot ulcers, or DFUs, are a common complication of diabetes, resulting from prolonged high blood sugar levels that damage blood vessels and nerves. This condition impedes wound healing and leads to ulcers in weight-bearing areas such as the ball of the feet, heels, and toes. These types of diabetic foot ulcers can have severe consequences, contributing to a significant number of hospital admissions among people with diabetes. To effectively manage and treat DFUs, podiatrists use classification and scoring systems that can provide valuable insights into the severity and potential complications of these wounds. One widely recognized classification system is Wagner's, which assesses DFUs based on six grades. Factors such as ulcer depth, tissue necrosis extent, and bone infection presence are examined. The results range from Grade 0, which indicates no open lesions, to Grade 5, which shows gangrene of the entire foot. Wagner's system aids in treatment planning and understanding ulcer severity. If you suffer from diabetic foot ulcers, it is suggested that you make regular appointments with a podiatrist to monitor the stages of the ulcers.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes affects millions of people every year. Blood vessels located all over the body are damaged due to diabetes—even the blood vessels of the feet. Neuropathy, or nerve damage, can result from slower blood flow in the legs and feet. In diabetic patients, neuropathy is very important to monitor, as diabetics are at risk for developing ulcers.
Always washing and thoroughly drying the feet are pertinent parts of diabetic foot care. There should be a focus on cleaning between the toes. Even if no pain is felt, the entire foot should be examined for redness and sores. Neuropathy can often mask the pain of sores and ulcers and can cause these conditions to be overlooked. Use a mirror to examine the underside of your feet if needed. It is recommended that diabetics wear well-fitting socks.
Patients with diabetes should have their doctor monitor their blood levels because blood sugar levels play a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised. It is very important to keep your blood sugar levels in the normal range, which can be determined by your physician. There are medications that may be prescribed to help with any neuropathy experienced by the diabetic patient. It is also advisable to visit a podiatrist if one is experiencing any conditions involving the feet, such as ingrown toenails, which in more severe cases can cause infection.
Diabetic feet must be inspected daily. Diabetic foot care at home is possible if a patient is provided with instructions from their podiatrist. Patients can relieve dry heels with creams or ointments. Suspected wounds should warrant an immediate call to the podiatrist. Gangrene is a serious problem for diabetics and can lead to sepsis and amputation in its worst cases. Early treatment and daily inspection of diabetic feet are keys to staying healthy.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
Are Bunions Affecting Your Everyday Life?
Causes and Solutions for Ingrown Toenails

Ingrown toenails, a common and often painful foot condition, can make each step a struggle. An ingrown toenail occurs when the edge of a toenail grows into the surrounding skin, causing inflammation and discomfort. Causes can range from improper nail trimming techniques to wearing tight shoes that exert pressure on the toes. In some cases, a genetic predisposition or an injury can trigger this condition. Soaking the foot in warm water, gently lifting the ingrown edge, and applying antibiotic ointment can aid in healing. Wearing open toed shoes and avoiding tight footwear can also promote recovery. Seeking medical attention for severe cases ensures effective relief, often involving minor surgical procedures to remove the ingrown portion. By addressing the root causes and following appropriate treatment, individuals can bid farewell to ingrown toenail discomfort and regain comfortable strides. If you have developed an ingrown toenail, it is suggested that you seek the counsel of a podiatrist who can guide you toward the correct treatment method.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Stretches for Better Ankle Mobility

Improving ankle mobility is vital for overall flexibility and performance, whether you're an athlete or simply seeking better movement. Strengthening and stretching exercises can prevent injuries, enhance walking posture, and maintain strong knee and hip muscles while alleviating ankle pain. Beneficial exercises include ankle circles, single-leg balances, and toe raises. Ankle circles involve rotating your ankle on a rolled-up towel or foam roller in clockwise and counterclockwise circles. For single-leg balances, stand with feet shoulder-width apart, arms out to the sides, while lifting one foot off the ground. Toe raises require standing on a step on the balls of your feet, rising onto your toes, and lowering the foot below step level. These exercises promote better movement awareness, reduce the risk of ankle sprains, and establish a strong, stable foundation. For personalized guidance, it is suggested that you consult a podiatrist to assess your feet and ankles and receive tailored care.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Ankle Pain
Pain experienced in the ankle can be caused by a multitude of conditions. While the most common cause is an ankle sprain, other possible problems can include arthritis, gout, ankle instability, an ankle fracture, nerve compression, or tendinitis. In more serious cases, ankle pain can be a sign of improper alignment of the foot or an infection.
Ankle pain can often be accompanied by symptoms such as redness, swelling, stiffness, and warmth in the affected area. Pain can be described differently depending on the condition: short, stabbing pain and a dull ache are some examples. If such symptoms are persistent and do not improve after time, be sure to schedule an appointment with your local podiatrist.
Depending on the condition causing your ankle pain, different treatments may be prescribed by your podiatrist. For ankle sprains, the first step in treatment involves rest, ice, elevation, and compression. Be sure to avoid placing pressure on the ankle, use an ice pack several times a day, and use a compression bandage and elevation to reduce swelling. Other, more serious conditions may require the assistance of certain drugs and medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, or even cortisone injections.
Depending on the severity of your ankle pain and the condition behind it, recovery from ankle pain may take some time.
Consult with your foot and ankle doctor to best determine the cause of your ankle pain and the appropriate treatment.